Risks and Benefits of Screening Tests, Part 2
By Deborah Bickel PA MPH
Why should an older adult think about all the diseases that might be their fate? Because these might happen in a few years or even a few days.
Years ago, people could do very little to prevent what they saw as fate or bad luck. As flawed as many find allopathic [or “western”] medicine, few can argue that it has advanced to a stage where we can find out what may be threatening our health or cutting short our lives. These are often done with simple, or, at times, more complex testing. Once we know the results, we can sometimes take measures to prevent or put off disease that would have taken us by surprise and killed us at an early age.
An important thing to remember is that the science and practice of screening is a first world phenomenon. We, unlike most human beings, live long enough and with enough surplus income to make these recommendations a reasonable expense for affluent societies. Even in the United States, many citizens can neither afford or access screening services and/or preventive treatment. US stands alone among “affluent societies where preventable death is radically higher depending on income and race….and some would say gender.”
A fact we all face is that with aging comes a greater risk for many more diseases associated with being alive beyond the 35 or 40 years allotted us historically. We can test blood, hearts, lungs, skin and bones with a wide variety of “screening” procedures that allow early detection and early treatment of disease that might once have killed us at an early age. That is not to say all this testing is an exact science. A good clinician will know what is necessary and what produces confounding or confusing results contributing to false signs of disease.
Some people have genetic predispositions or diseases that make earlier screening even more useful. A good clinician should be able to advise you on what tests give you useful information about prevention of early onset of many diseases from cancer to heart disease, blindness, strokes and even some kinds of dementia. This article is meant to help you decide what you could or should test for, and this knowledge may even educate your doctor along the way.
Remember, screening isn’t as common a concept in Mexico as it is in the U.S., and you may need to take the lead. Be Well advocates can also advise you on what you should be testing for and help you find a doctor willing to do it.
*NOTE: These recommendations come from the US Preventive Services Task Force an independent expert body that makes recommendations to the government and medical organizations in the US. It is independent from any commercial interests.

RECOMMENDED SCREENING TESTS FOR OLDER ADULTS.
Blood Pressure
Everyone, starting in the late teen years and even younger children at risk of obesity should get blood pressure screening.
Blood Chemistry Screening
A CBC or complete blood count looks at white and red blood cells.
A metabolic panel checks levels of enzymes (substances that speed up chemical reactions), electrolytes such as sodium and potassium, proteins and blood sugar. It is also used for people with blood clotting disorders, diabetes, kidney or liver disease, to look for drug side effects or before major surgery.
Cholesterol Screening
Cholesterol is a fat as well as a protein. Testing looks at all types of fats or lipids in the blood. It is important to understand that some types of cholesterol are protective of heart disease. These are called high density lipoproteins or LDL. The dangerous ones or those associated with increased heart attacks and strokes are the low-density types along with triglycerides or fatty acids. Total cholesterol above 240 and LDL above 190 increase the risk of heart attacks and strokes.
Adults 40 to 75 years old with one or more cardiovascular risk factors such as smoking, family history, drinking or diabetes should be checked every 5 years. If results are outside healthy range, testing should be more frequent. People under 40 with a family history of early heart disease should be screened at least once.
One of the most common drugs prescribed in the developed world are cholesterol-lowering drugs. Some say they are prescribed too frequently before other measures are taken such as diet and exercise. A healthy person over 75 may or may not want to test their cholesterol and lipids, depending on overall health status. Although it is not recommended, testing lipids and treating mild abnormalities in those over 75 is a booming business for the healthcare industry.
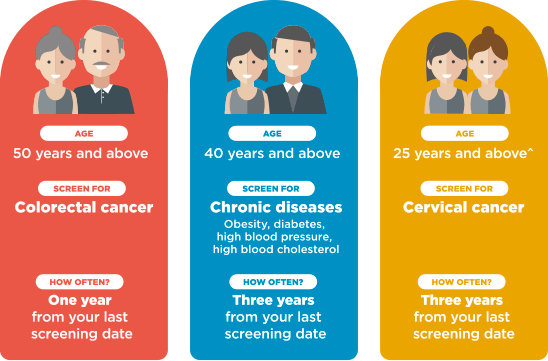
Colorectal Screening
There is a new test that can be done on stool that looks for the DNA related to cancer (not just presence of blood, as older tests do). If this test is negative, the chances of you having a cancer or precancerous condition are pretty slim. If it’s positive, it still doesn’t mean there’s cancer, it just means you need to get a colonoscopy to view the entire lower bowel. Colonoscopy is the gold standard, but it is not an entirely benign test. For example, for those with heart disease it is best to have the procedure in a setting where an emergency room or urgent care doctor can respond immediately. Those on anticoagulants need to taper off them in a carefully designed fashion before surgery.
The recommendation for starting screening is 50 years old, but recently there have been more colorectal cancers found in younger populations and recommendations have moved to 40 years of age. The general recommendation is screening with colonoscopy once every 10 years unless polyps and other abnormalities have been found in the past. The cancer detecting stool samples are recommended every one to two years. The older we get, the more risk is involved in a colonoscopy. Looking for the cheapest procedure often means there is no support for cardiac emergencies or a perforated bowel. This is not a place to cut corners by choosing the cheapest site offering colonoscopies. People over 76 should talk to their doctors about whether the risk outweighs the benefit.
Screening for Bone Density and Strength
This is usually done with low dose X-ray. The task force suggests one-time screening for women 65 or older unless they had an early menopause or other risk factors. They recommend no screening for younger women unless they have taken some types of drugs or had various diseases that put them at risk. Screening for men is recommended at age 80. If bones are weak or brittle, extra precautions to avoid falls can be taken. There are those that say weakening bones are not a disease but merely a natural result of aging. Calling it a disease is a way of pathologizing normal processes. This is true, but we live far longer and many practical measures can be taken to avoid broken bones and the disability they cause.
Hepatitis C Screening
Anyone who had a blood transfusion from 1945 to 1965 should be screened for Hepatitis C. The virus was not identified until after 1965. Hepatitis C is a blood-borne disease, and health workers should be immunized. It is also a sexually transmitted disease. It is usually symptomless and can clear on its own in 15 to 25 percent of those with the virus. If it does not clear, it can lead to cancer and severe liver disease, OFTEN with no symptoms. Antiretroviral therapy is available that clears the disease in 90 percent of the cases. There are programs to distribute the drug at low cost to poorer clients in the US and Canada, and everyone should consider treatment in order to avoid cancer, liver transplants and liver disease. The disease is made worse by drinking alcohol. Remember, you may have no symptoms at all, so it is best to be screened.
Abdominal Aortic Aneurysm Screening
This is recommended for men 65 to 75 who are current or former smokers. There is a good argument that women who are former smokers should also be screened.
Non smoking men and women 65 to 75 who have never smoked might consider the test if they have a family history. Aortic aneurysms are deadly a great deal of the time.
EKG and Stress Testing
These are only recommended for those at risk of heart disease, such as those with strong family histories. Done on the general population it can lead to invasive testing and unnecessary procedures. Those “executive screening plans” nearly always recommend EKGs and stress testing for the general population. It is a money maker and many have the false notion that they are necessary every year and can free them of any cardiac concerns. EKGs and stress testing are notorious for leading to more invasive testing such as angiography or angioplasty. Both of these procedures carry cardiac risk, angioplasty in particular.
Carotid Artery Screening
This is done by an ultrasound at each side of the neck. The test is looking for narrowing of the arteries that can lead to strokes. This is done by a skilled technician or physician for anyone who has symptoms of a stroke or transient ischemic attack (TIA), sometimes called a mini-stroke. Only one percent of the population has severe narrowing of the arteries, and even these seldom lead to stroke unless there are other risk factors such as high blood pressure or some kind of cardiac diseases. Most experts recommend against routine screening as it often leads to unnecessary high-risk procedures.
Heart Scans
Heart scans are otherwise known as Coronary CT angiography (CCTA). A second scan is called CCTA use multiple x-ray images of the heart.
These tests are only recommended for those with cardiac symptoms such as shortness of breath, chest pain and those at a high risk for heart disease such as diabetics or those with a strong family history of cardiac death at a young age. These tests are not commonly recommended and the society of Computed Tomography advise against their use for the general population.
Lung Cancer Scan
These scans have found lung cancer early and can prevent death from the disease. The US Preventative Services task force says: Adults 55 to 80 with a history of smoking one pack a day for 30 years or two packs for 15 years should be screened yearly. Unfortunately, only 2% of those who should be screened get screened. This is partly because the test is expensive and has a lot of false positive findings. For every lung cancer death prevented, 302 people without the disease have positive findings. That is an example of a false positive test. (2013 USPFTF)
Mouth and Neck Screening
This is done to check for cancers or precancerous growths such as lesions of papilloma virus. Papilloma virus can lead to cancer. Despite the ease of the exam by dentists and general practitioners, it is not recommended for healthy people. If there is a history of smoking or heavy drinking, exams are indicated as these increase the possibility of cancers. The rational is that most lesions are benign and if all were biopsied there would be a lot of false positives.
Full Body CT Scans
These are radiologic exams of the entire body and thus expose the patient to more radiation than nearly every other test except a PET scan. (PET scans are often used to look for metastases of cancer). CT scans are notorious for finding results that at first appear abnormal or alarming and then once more testing is done are found to be common anomalies. No one body is identical to the next and human variation is often unaccounted for. Almost worse for the patient is a false positive CT scan that leads to follow up scans exposing the person to even more radiation.

Mammograms
There is controversy among the various panels recommending the testing. The age range is 40 to 45 and 50. There is a fair amount of radiation in routine mammography and some women opt for MRIs which have no radiation. The downside is that MRIs find a lot of false positive signs and can lead to unnecessary surgery and worry. There is a trend toward digital mammography which translates the x-rays into electronic impulses that can be analyzed by computers as well as humans. Women with dense breasts (usually this is a finding on mammograms and density is technically rated) may want to have MRIs or digital mammograms or even routine mammograms more frequently than current recommendations. There are no digital mammograms in San Miguel de Allende. There is an MRI at CEII behind UNIMED.
Screening after 75 is probably unwarranted as cancers grow slowly in older women. Of course, if there is a history of earlier breast cancer screening is imperative. MRIs do find more cancers but there is no evidence that they save lives.
Pap and HPV screening
Some sub-types of human papilloma virus (HPV) are strongly associated with cancer.
The Pap smear looks at cervical cells for any precancerous lesions and the presence of HPV or human papilloma virus. Some subtypes of HPV are strongly associated with cervical cancer. Mexican women have a very high rate of cervical cancer related to a high rate of cancer-causing HPV. A public health campaign to immunize young people against HPV has been very hard to get off the ground given religious and cultural mores around sexuality.
The recommendation is that women from 21 to 29 should have Pap smears every three years. Older women up to 65 can follow the same recommendation or spread it out to five years unless they have had abnormal Pap smears in the past. Women who have had hysterectomies that removed the cervix and have never had reproductive tract cancer do not need Pap smears
Mexican women may want to have pap smears yearly if they are sexually active.
Prostate testing (PSA)
This has become a controversial issue. PSA is often elevated in prostate cancer, but it is also elevated after sex, after a rectal exam or vigorous exercise, or can be due to an enlarged prostate and very mild non aggressive cancers. Its main use is to monitor those who have already had aggressive prostate cancer. A good physician will discuss the risk and benefits of screening, but patients should steer away from any clinician using it as a screening tool for those who have never had prostate cancer. The bottom line is that the male consumer should understand that a high PSA rate can lead to unnecessary surgery or radiation in the absence of cancer. There is a growing understanding that PSA testing should be used sparingly and is not a screening test at all. Many cancers were detected in the heyday of PSA screening but very few lives were saved and significant disability resulted as a result of surgery such as bowel problems and impotence. Increasingly non-aggressive cancers are being identified and simply monitored for any changes.
Digital rectal exams are also falling by the wayside. The enlarged prostate inherently has lumps and bumps that may mean nothing. However, the exam is non- invasive and there is really no other screening test for prostate cancer.
Skin Cancer Screening
Many doctors aggressively burn or cut away cancers or precancerous lesions when in fact leaving them alone may be the best route for management. The yearly skin screening should be looking mostly for melanomas, the most dangerous of cancers, as well as basal cell cancers that can spread and enter deeper tissue. One fact many may not know is that sun screen does not prevent melanomas. You should be familiar with the moles and lesions on your body and see a dermatologist if there is any change. Some dermatologists do yearly skin checks on those with fair skin or many moles and photograph them in order to identify any future changes. Any nodule or raised area of skin that bleeds, itches and refuses to heal should be checked by a dermatologist. These are the signs of basal cell carcinoma.
Thyroid Screening
Now days it is done by ultrasound when they are available. Palpation can pick up abnormalities as well but not as precisely. Most irregularities are non-cancerous or very slow growing cancers. Those who should seek ultrasound are those who have been exposed to a lot of radiation such as radiation therapies for other cancers. If an abnormality is found, discuss with your doctor the risks and benefits of doing anything about it aside from monitoring.
Type 2 Diabetes
There are two common tests: one is a fasting blood sugar and the other is called a hemoglobin A1C which detects elevated glucose over about three months. There is controversy as to who should be screened. Certainly, if you are over 45, overweight, have a family history of diabetes and lead a sedentary life style testing will be recommended. Those over 45 with no risk factors should be screened as a matter of course. If tests are normal, retest every three years and those who are at the border every one to two years. If prediabetes is diagnosed, every effort should be made to manage it with diet and exercise rather than medication, which can make it harder to lose weight and return your glucose to a normal level. Never simply start with a medication because someone told you were “prediabetic”. Use it as a time to take a look at lifestyle and diet.
For more information, contact Deborah Bickel, PA MPH at
Deborah@bewellsanmiguel.com 415-1157815